It was the fall of 2013 and Autumn Paolini was in her 10th grade year at Neshannock High School when her appendix ruptured. She was taken to a hospital near her hometown of New Castle, Pa., for an emergency appendectomy.
She made it through the surgery, but not without complications. She was in the hospital for two weeks afterwards due to an abscess in her abdomen that had formed post-surgery and wasn’t allowing her to go to the bathroom.
At that point, she was taking medications regularly to help her continue to heal and her doctors felt that it would be beneficial for her to have a peripherally inserted central catheter – or PICC line – inserted. The PICC line would help to ease the administration of the medications. Doctors referred her to UPMC Children’s Hospital of Pittsburgh to have the PICC line inserted.
Autumn had lost a significant amount of weight, but she continued to heal and was able to resume her school year.
Stress Headaches, Migraines, or Something Else?
In April 2014, Autumn began experiencing frequent headaches. When the headaches didn’t subside for a week, Autumn and her family decided to get an opinion from another doctor in town.
That doctor thought the headaches may be stress related. Within a matter of months, Autumn been through a major surgery, experienced complications and extreme weight loss, and had returned to school and playing softball. This seemed reasonable to the Paolinis who returned home and continued to monitor the frequency of Autumn’s headaches.
By week two of the headaches, they had become progressively worse and longer. She also began having vision problems. The family was in communication with the doctor who had asked if the headaches kept Autumn up at night. They didn’t at the time so the doctor determined that scans weren’t in order at that point.
By week three, the headaches were constant and so painful that Autumn couldn’t turn her head.
Autumn’s family took her to the local Emergency Room where she had a CT scan.
When doctors examined the images, they saw a mass in the center of Autumn’s brain.
A Transfer to Pittsburgh for Life-Saving Surgery
 Autumn was immediately flown by medical helicopter to UPMC Children’s. Doctors there determined that she had hydrocephalus along with a mass that was a tumor.
Autumn was immediately flown by medical helicopter to UPMC Children’s. Doctors there determined that she had hydrocephalus along with a mass that was a tumor.
Hydrocephalus is sometimes known as “water on the brain,” but is more accurately described as a buildup of cerebrospinal fluid (CSF) that can cause pressure inside the head to increase. This pressure was causing Autumn’s painful headaches.
The tumor was located in the third ventricle – a central space in the brain containing CSF.
Before doctors could address the tumor, they needed to address the hydrocephalus.
Autumn was quickly scheduled for brain surgery with Stephanie Greene, MD, pediatric neurosurgeon at UPMC Children’s. Dr. Greene is director of Vascular Neurosurgery and director of Perinatal Neurosurgery.
Dr. Greene would insert a ventriculoperitoneal (VP) shunt into Autumn’s brain. A VP shunt is a device used to help drain the extra CSF from the brain and redirect the extra fluid to another part of the body. For Autumn, the CSF would be directed to her abdomen where it would be absorbed into the bloodstream and filtered out through the kidneys.
Insertion of the VP shunt is done under general anesthesia, which at UPMC Children’s is administered by pediatric anesthesiologists who specialize in treating children. During the surgery, Dr. Greene was also able to take a biopsy of the tumor for further evaluation.
The surgery was successful and afterward, Autumn reported that the headaches had completely gone away. With the immediate concern of the hydrocephalus addressed, it was time for doctors to learn more about her tumor to figure out how best to treat it and prevent the hydrocephalus from returning.
A Diagnosis and a Trial
 The biopsy of Autumn’s brain was sent to the lab to learn more about what they were dealing with.
The biopsy of Autumn’s brain was sent to the lab to learn more about what they were dealing with.
“We didn’t know if it was cancerous or metastatic (the process by which cancer cells spread to other parts of the body),” says Autumn. “But the only positive thing we did know was that they had done a CT scan on my spine as well and there was nothing in the spine. So that gave us some hope.”
Autumn vividly remembers the day Dr. Greene called with the biopsy results. The family had gone grocery shopping and she, her mom, and her dad were carrying the bags in when her mom took the phone call. Her mom had started to cry and Autumn turned to her dad saying, “Dad, tell mom to stop crying all the time!” It had been an emotional few months for her family, to say the least.
Dr. Greene reported to Autumn’s mom that the tumor was a low grade juvenile pilocytic astrocytoma (JPA). JPAs are rare childhood tumors that are usually slow-growing and do not usually spread to surrounding brain tissue. Pilocytic refers to the fact that the tumor is made up of cells that look like fibers – or as Autumn describes it, “like a web” – when viewed under a microscope.
“It was not like a neat circle or mass where you can pick it up and move it,” explains Autumn. “It was also centrally located and right on the optic nerve, so it was determined that it was inoperable. So we had a diagnosis, but we needed to look into non-surgical treatment options.”
 Autumn was referred to Gary Mason, MD, who was then director of Neuro-Oncology at UPMC Children’s. The team started Autumn on Carboplatin infusions. Carboplatin is considered the “gold standard” of chemotherapy for low-grade tumors. It is often the first choice for treatment when tumors are not resectable, like Autumn’s. The team decided against radiation at that point because of her age. She continued the Carboplatin infusions for 10 months, but the tumor was still growing.
Autumn was referred to Gary Mason, MD, who was then director of Neuro-Oncology at UPMC Children’s. The team started Autumn on Carboplatin infusions. Carboplatin is considered the “gold standard” of chemotherapy for low-grade tumors. It is often the first choice for treatment when tumors are not resectable, like Autumn’s. The team decided against radiation at that point because of her age. She continued the Carboplatin infusions for 10 months, but the tumor was still growing.
Even though she was scheduled to be on Carboplatin for a full year, Autumn says, Dr. Mason could see it was not working. “[He] said ‘We’re going to stop and try something else.’ I felt like he was listening to me and didn’t want to waste any time on treatments that weren’t working.”
UPMC Children’s was a founding member of the Pediatric Brain Tumor Research Consortium (PBTC) which was, at that time, studying a new approach to these tumors using an oral medicine called selumetinib. As a member of the consortium, Dr. Mason was aware of the selumetinib trial, then in Phase II, and that many of the participating patients who had very similar tumors to Autumn’s had experienced positive preliminary results. Many of the participants even had the exact same B-RAF mutation as Autumn, and their tumors were shrinking.
“It seemed promising, but the issue was that with studies and trials, they’re not approved by the FDA (U.S. Food and Drug Administration) yet. And there are only so many slots available and none of them were open at the time,” said Autumn.
There is generally less funding for pediatric research than for adult research, which can make trials hard to come by. But the very next month, two slots did open up in the selumetinib trial, and Autumn was able to take one of them.
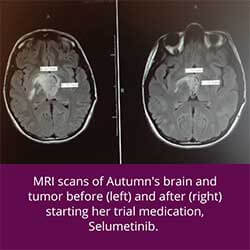
As part of the trial, Autumn would receive the medication monthly and she would come in for MRIs every three months to monitor the tumor. Her very first MRI showed that her tumor had shrunk to half the size.
“It was an amazing response from just the first three months,” says Autumn. “I could tell too just because of how my body felt that it was a positive response.”
After nine months on the medication, the tumor shrunk a bit more and then stabilized. The goal with inoperable tumors like Autumn’s is to stabilize them, not necessarily eliminate them completely. She continued on the selumetinib trial for two years until that arm of the trial was complete. At that point, she had graduated from high school and Dr. Mason had left UPMC Children’s. Autumn’s care was transferred to the new director of Neuro-Oncology, Alberto Broniscer, MD, MS.
Around this time, Autumn went off her medicine for about three months. She immediately began having symptoms again. Her tumor began to grow and she started to accumulate fluid in her abdomen – a condition known as ascites. That summer, she had to have her abdomen drained three different times. At one point, two liters of fluid were removed.
Autumn and her care team carefully weighed whether she should try to get back on a different arm of the selumetinib trial or perhaps try to take part in a different trial. They ultimately decided it would be best to try the selumetinib again and were able to get her a spot in part C of the trial.
Sure enough, once Autumn was back on the medicine, the ascites went away and her tumor stopped growing.
What’s Next for Autumn
 Nowadays, Autumn still has her shunt in place and is still participating in part C of the selumetinib trial. For five and a half years now, she has taken the medicine each morning and night and her tumor has stabilized.
Nowadays, Autumn still has her shunt in place and is still participating in part C of the selumetinib trial. For five and a half years now, she has taken the medicine each morning and night and her tumor has stabilized.
She has experienced a few mild side effects from the medicine – her hair has changed colors because of the medicine on her hair follicles, and she has experienced some acne – but nothing that has outweighed the benefits of the medicine on her maintaining her quality of life.
The FDA has approved selumetinib for the treatment of other illnesses, but not yet for Autumn’s specific tumor. Because of the success she has had in stabilizing her tumor while on the medicine, she is hoping that this will change once the trial concludes.
Autumn, who is now almost 25 years old, visits Children’s every three months for a check-up and scans to monitor her tumor. Even so, Autumn says she has “never disliked a visit because of the environment and everyone is so nice.”
“All of my doctors have been nothing but welcoming and caring. They’re kind of like family, you know?” said Autumn. “And, Sharon, who is a research coordinator in the neuro-oncology department, has been like a mom to me. She helps to keep me up-to-date and helps me schedules appointments. It’s so personal. Nobody was ever rushing you out of the door. I know some people hate going to the doctor, but I’ve truly never felt that way at Children’s.”
Because the tumor is “juvenile,” there is a chance that it will stop growing on its own after a certain point and the medicine may not become necessary. Until then, she hopes she will be able to continue taking it.
“I’m very much back to living a ‘normal’ life,” says Autumn. “I am blessed to have the doctors that I did at Children’s that helped to get me on my medicine and helped me get back to that ‘normal’ life. Most people wouldn’t know by just looking at me now what I’ve been through and am still dealing with. That’s why I feel it’s important to share my story. I’m grateful to be here and I just want to help and pay it forward.”
By the same token, Autumn wants people to know your obstacles shouldn’t define you.
“It’s so important to make the most of every day. And that’s what I’ve been doing. I’m not letting my tumor define who I am. I have so many other things going for me,” says Autumn.
And she’s right.
Autumn earned her high school diploma, bachelor’s degree in chemistry, and her master’s degree in teaching, all while dealing with her health challenges.
When she started her college career, she thought she wanted to become a physician assistant because of the “awesome PA” she had at Children’s. After two years, she decided to be a high school chemistry teacher – a career choice she says was equally impacted by all of her experiences.
 She now has a job teaching high school chemistry and even has her own small confectionary business where she can be found whipping up dozens of cake pops in her spare time.
She now has a job teaching high school chemistry and even has her own small confectionary business where she can be found whipping up dozens of cake pops in her spare time.
When asked what her advice to others in a similar situation would be, Autumn said: “I wouldn’t be here without my mentality: You can’t give up. You have to have strength and believe. I’ve always been of that positive mindset. Challenges aren’t there to break you, they’re there to make you grow and to help you get stronger. For me, it’s rooted a lot in religion and God. God can get you through anything. We’re all here for a reason. I got through this because there’s something bigger in my life coming down the road.”









