After the flexible bronchoscopy, your child might feel tired for several hours and might have a sore throat, a cough and/or some blood in his or her saliva (spit) when he or she coughs. These should go away by the next day. If they don’t, you should contact the doctor’s office.
About half of the children who have had a bronchoscopy with bronchoalveolar lavage (BAL) will develop a low-grade fever 4 to 8 hours afterward. This fever is a normal response of the body and can be treated with Tylenol®. If your child develops a fever that is higher than 102.5 degrees F or 39.1 C, or does not respond to Tylenol, you should call the hospital and ask for the pediatric pulmonologist on call.









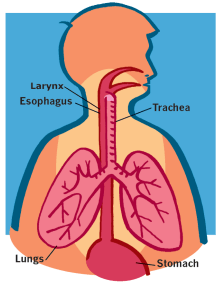 In a bronchoscopy (bron-KOS-ka-pee), a long flexible tube with a tiny camera, called a bronchoscope (BRONK-a-scope), is passed through the nose or mouth into the lungs. The doctor can see what the vocal cords, trachea (TRAKE-ee-uh) and the airways in the lungs look like.
In a bronchoscopy (bron-KOS-ka-pee), a long flexible tube with a tiny camera, called a bronchoscope (BRONK-a-scope), is passed through the nose or mouth into the lungs. The doctor can see what the vocal cords, trachea (TRAKE-ee-uh) and the airways in the lungs look like.
