- Find a Doctor
-
For Parents
- Before Your Visit
- During Your Visit
- After Your Visit
- More Resources for Parents
Patient & Visitor Resources -
Services
- Locations
-
About Us
- About Childrens
- Find it Fast
- Additional Resources
Find it FastAdditional Resources - MyCHP
ALERT:
There is construction in and around UPMC Children’s Hospital that is affecting the traffic flow – please allow for extra time traveling into the hospital.
- Find a Doctor
- For Parents
-
Services
-
Frequently Searched Services
- Asthma Center
- Brain Care Institute (Neurology & Neurosurgery)
- Cancer
- UPMC Children's Express Care
- Ear, Nose, & Throat (ENT)
- Emergency Medicine
- Endocrinology
- Gastroenterology
- Heart Institute
- Genetic & Genomic Medicine
- Infectious Diseases
- Nephrology
- Newborn Medicine
- Primary Care
- Pulmonary Medicine
- Rheumatology
- Surgery
- Transplant Programs
- See All Services
-
Frequently Searched Services
- Locations
- About Us
- MyCHP
- I Want To
- More Links









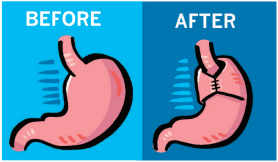

 If your child had the laparoscopic procedure, he or she will have Steri-StripsTM covering the small incisions. Steri-Strips are adhesive strips that are sometimes used on shallow cuts instead of stitches to hold the edges of the cut together. They will dry up and fall off on their own as the incision heals.
If your child had the laparoscopic procedure, he or she will have Steri-StripsTM covering the small incisions. Steri-Strips are adhesive strips that are sometimes used on shallow cuts instead of stitches to hold the edges of the cut together. They will dry up and fall off on their own as the incision heals. Your child also should avoid eating certain foods.
Your child also should avoid eating certain foods.