Pectus (PEK-tuss) is a Latin word that means “chest,” and excavatum (ek-ska-VAT-um), also Latin, means “caved in.”
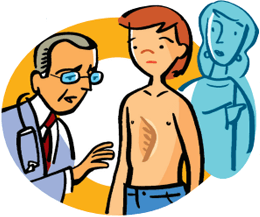
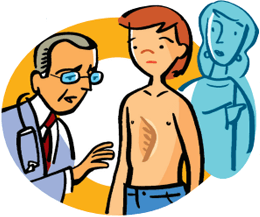
The ribs are attached to the bone in the middle of the chest called the sternum (or breastbone) with cartilage (KART-il-ij). Cartilage is soft, flexible tissue. Pectus excavatum, also called “funnel chest,” is a condition that occurs when this cartilage overgrows onto itself, causing the sternum to curve inward, making the child’s chest look as if it has been “pushed in.”
When this condition occurs, the heart is pushed from the “midline,” or center of the chest, and rotated to the left side of the chest, possibly affecting its ability to pump blood. When the heart can’t pump blood the way it should, the child may get tired quickly during exercise. The curve of the sternum also may cause a squeezing effect on the lungs, making it harder to breathe.
- Pectus excavatum is the most common chest wall problem in children.
- Pectus excavatum occurs mostly during the early teenage years in times of rapid growth, and mostly in boys.
- Surgical repair may be done to fix breathing and heart problems, but it may also be done for cosmetic reasons—to make the chest look normal.
The surgery is elective, meaning it can be done when parents want to schedule it. Many choose to have their child’s surgery during the summer to allow their child more time to heal without missing school.
The surgery is done under general anesthesia (an-es-THEEZ-ya). General anesthesia makes your child’s whole body go to sleep and is needed for this surgery so that his or her reflexes will be completely relaxed. General anesthesia makes the surgery easier and safer to do because your child will not feel any pain or have any memory of the surgery.